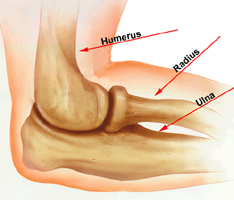
 Our elbow joint is made up of bone, cartilage, ligaments and fluid. Muscles and tendons help the elbow joint move. When any of these structures is hurt or diseased, you have elbow problems.Our elbow joint is made up of bone, cartilage, ligaments and fluid. Muscles and tendons help the elbow joint move. When any of these structures is hurt or diseased, you have elbow problems.
Our elbow joint is made up of bone, cartilage, ligaments and fluid. Muscles and tendons help the elbow joint move. When any of these structures is hurt or diseased, you have elbow problems.Our elbow joint is made up of bone, cartilage, ligaments and fluid. Muscles and tendons help the elbow joint move. When any of these structures is hurt or diseased, you have elbow problems.
Many things can make your elbow hurt. A common cause is tendinitis, an inflammation or injury to the tendons that attach muscle to bone. Tendinitis of the elbow is a sports injury, often from playing tennis or golf. You may also get tendinitis from overuse of the elbow
The injuries around the elbow will be described under the following heads:
- Fractures of the distal end of the humerus
- Dislocation of the elbow
- Fractures of the proximal ends of the radius and ulna.
- Supracondylar fracture
- Intercondylar fracture
- Fracture of the lateral epicondyle
- Fracture of the medial epicondyle
- Fracture of the capitellum.
Supracondylar Fracture Of The Humerus
Supracondylar fracture of the humerus is one of the most common fractures in the children, and occurs in the age group of 3-13 years.
Mode of Injury
This fracture is caused by a fall on the outstretched hand.
Displacements
The fracture line runs transversely just above the condyles of the humerus. On the basis of the displacements, fracture is classified into two types:
- Extension type: In this type the distal fragment is displaced posteriorly.This is the most common type and discussed here.
- Flexion type: In this rare type, the fragment is displaced anteriorly. Most of the fractures are displaced fractures. In an extension type the distal fragment is:
(i) Displaced posteriorly
(ii) Tilted posteriorly
(iii) Titled medially
(iv) Internally rotated.
Clinical Features
The child complains of severe pain and swelling in the elbow following a history of fall. The child holds the elbow in a flexed position and resists any movement to the elbow. When brought early, the swelling is less and the following signs can be elicited:
- There is tenderness over the distal end of humerus,
- Crepitus can be elicited, although it causes pain and therefore should be avoided,
- Since the fracture line is above the condyles, and the whole of the distal end of humerus carrying the elbow joint is displaced backwards, normal three bony point relationships is maintained.
When presented late, gross, tense swelling sets in which fills up the hollows around the elbow and obscures the bony landmarks. Sometimes even blisters develop over the elbow. In such a situation the fracture signs cannot be elicited. At the time of injury the distal fragment is displaced posteriorly there by pulling the brachial artery and the median nerve against the sharp distal end of the proximal fragment. This may cause injury to the brachial artery and/or the median nerve. It is therefore important to feel the radial pulse and test the nerve functions at the time of initial examination and make a record of it.
If the distal circulation is affected due to an arterial injury, the following features (5 Ps) may be seen:
- Pain- severe
- Pallor
- Pulselessness
- Paraesthesia, and
- Paralysis.
Investigations
Anteroposterior (AP) and lateral view radiographs of the elbow are essential. The AP view shows the fracture line which runs transversely just above the condyles. The distal fragment is displaced and rotated. The lateral view shows the posterior displacement of the distal fragment.
Treatment
An undisplaced fracture is treated above-elbow PoP slab for 3 weeks. A displaced fracture can be treated by one of the following methods:
- Closed reduction: The fracture is reduced by closed manipulation under general anesthesia. The reduction is obtained by gentle traction to the forearm, manual manipulation of the fragments to align them properly, and then flexing elbow a little beyond 90°. If the radial pulse becomes feeble or disappears during flexion of the elbow, then the elbow is extended gradually till the pulse reappears. The fracture is then immobilized with the elbow in the same position. The fracture may be stabilized by passing.
K-wire percutaneously. The extension type of the fracture is immobilized in an above-elbow PoP slab with the elbow in flexion, whereas the flexion type (less common) of the fracture is immobilized with the elbow in extension. In either case, the plaster is removed after 3 weeks.
- Traction: The cases which report late (more than one week) with marked swelling and blisters etc. are treated by continuous (Dunlop) traction for 3 weeks.
- Open reduction: Open reduction of the fracture is indicated when:
- The closed manipulation fails,
- The brachial artery is injured and needs exploration, and
- There is an associated nerve palsy which needs exploration.
- After open reduction the fracture fragments are fixed internally with Kirschner wires-(commonly called K-wires)
Early complications
These complications occur at the time of injury immediately after.
1. Injury to the brachial artery: This is the most dreaded complication; the brachial artery is injured by the sharp edge of the proximal fragment. The artery may actually be lacerated, thrombosed or may just go into spasm. The blood supply to the flexor muscles of the forearm may be affected resulting into Volkmann’s ischaemia. This requires immediate treatment.
Volkmann’s ischemia: Injury to the brachial artery leads to impairment of circulation to the forearm and hand. There occurs ischemia of the deeper muscles of the flexor compartment of the forearm, such as flexor pollicis longus and flexor digitorum profundus. The muscle ischemia, in turn, leads to compartment syndrome.
Diagnosis:
- There is severe, sudden increase in pain in the forearm
- Stretch pain.
There is severe pain in the flexor aspect of the forearm when the fingers are passively extended. This is the most important test and is pathognomonic of muscle ischaemia.
Treatment: The case of Volkmann’s ischaemia must be handled as an absolute emergency because changes may soon become irreversible.
- Remove tight bandage/splints/plasters etc. immediately.
- The forearm is elevated and hot bottles are applied to the other three limbs to promote general vasodilation.
- If no improvement occurs within 2 hours, the operation of fasciotomy is undertaken, if the flexor compartment is tight. In this operation an incision is made from skin down to the deep fascia to decompress the compartment.
- If the injury to the brachial artery is established by angiography/Doppler, exploration of the brachial artery is undertaken.
2. Injury to the nerves: Median, radial and ulnar nerves may be injured, in that order. In majority of the cases the nerve palsy recovers spontaneously.
Late complications
- Malunion: Malunion is the most common complication of supracondylar fracture of the humerus and results in a cubitus varus deformity. This deformity occurs if the fracture has been allowed to unite with appreciable medial and internal rotation of the distal fragment.
- Treatment: If the deformity is unacceptable cosmetically, a corrective osteotomy in the supracondylar area is performed (French osteotomy).
- Myositis ossificans: Myositis ossificans is ectopic new bone formation around the elbow. This is a common complication which occurs following massage to the elbow after the injury and results in stiffness of the elbow.
Volkmann’s ischaemia contracture (VIC): Volkmann’s ischaemia, if not treated in time, gradually progresses to Volkmann’s ischaemia contracture.
The ischemic muscles are gradually replaced by fibrous tissue, which contracts and draws the wrist and fingers into flexion. If the peripheral nerves are also damaged by ischaemia, there will be sensory and motor paralysis in the forearm and hand.
Diagnosis: There is marked atrophy of the forearm muscles. There is the characteristic deformity of flexion of the wrist and fingers.
Volkmann’s sign: This sign is characteristic of VIC where the fingers cannot be fully extended passively with the wrist extended: but when the wrist flexed, the fingers can be fully extended passively. This happens because the shortened/contracted flexor muscle-tendon units do not permit full extension of the fingers and wrist simultaneously.
Treatment: In established cases to normal is impossible because irreversible damage has occurred to the import and nerves. However, reconstructive surgery can only improve some function of the hand.
- Mild cases can be treated by:
(i) Stretching exercises by a physiotherapist and also by the use of
(ii) Turnbuckle splint which gradually stretches the contracted muscles.
- Moderate cases require a muscle slide surgical operation where the flexor group of the muscles is released from their origin from the medial epicondyle of the humerus and ulna.
- Severe cases can be treated by shortening of the forearm bones, proximal row carpectomy and wrist arthrodesis etc.
Considerations
Even after the fracture has healed, full motion of the elbow may not be possible. In most of these cases, the patient cannot fully straighten his or her arm. Typically, loss of a few degrees of straightening will not have an impact on how well the arm will work in the future, including for sports or heavy labor. So treat your problem of Elbow Injury with Physical Therapy. Physical Therapy is the best treatment for the Elbow Injury.