Types, Causes, Symptoms And Treatment of Muscle Injuries (Strain):
Definition of Muscle Injury:
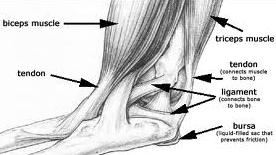
Injury to the muscle and tendons is called strain.
Reasons
- Sudden unaccustomed or abrupt action or movements may tear the muscles.
- Direct trauma can also injure the muscles and tendons.
- Overstretching of muscles due to indirect trauma, especially in sports persons.
Types
- Acute Strain: This is due to sudden violent force or direct trauma.
- Chronic Strain: This is due to injury existing since a long period leading to muscle ischemia and fibrosis.
Path physiology
Injury to the muscles leads to pain. As a result, the muscle goes into spasm to limit the movements and reduce pain. Nevertheless, paradoxically, this protective muscle spasm causes pain due to stimulation of pain fibers and thus a vicious cycle sets. The painful stimuli cause muscle spasm through the peripheral nociceptive stimuli.
Severity of Strain
- First Degree Strain (Mild Con Tusion)
- This is due to blunt injury and is due to direct trauma of lose intensity.
- Pathology: Few muscle fibers torn. Bleeding is minimal and the fascia remains intact.
Clinical Features
- Localized pain and tenderness.
- Pain and spasm prevents muscle stretching.
- Function is not impaired largely.
- Tenderness over the affected muscles.
Management:
- First aid is by Cryotherapy (by application of ice) for a period of 20 minutes.
- Gentle active muscle stretch may be permitted after 20 to 60 minutes.
- Compression bandaging with optimum pressure.
- Low dose and low power ultrasound helps.
- Gentle massaging of the surrounding area helps.
- If pain is minimal, the patient can be allowed to do the light work the next day.
Second Degree Strain
Cause: Here the trauma is more serious.
- Pathology
- Greater number of muscle fibers is torn.
- There is bleeding.
- The fascia is still intact.
- Hematoma is still localized.
Symptoms: Here are the symptoms.
- Pain is more severe.
- Tenderness is severe.
- Severe muscle spasm.
- The patient is unable to move the limb.
Third Degree Strain
Cause: Undoubtedly, these injuries are due to trauma of a greater magnitude.
Pathology: Larger area and greater number of muscle fibers are involved. More than one muscle group may be involved. The fascia is partially torn.
Bleeding is widespread and more. There could be both intramuscular and inter muscular bleeding. The patient experiences severe pain and loss of function.
Symptoms: Here all the above symptoms are of greater intensity.
Treatment in Grade II and III Strains
- For first 24 hours
- Immediate application of ice.
- Compression bandage.
- Limb elevation.
- Limb immobilized in splints.
- Isometrics to the muscles, which are immobilized.
- Active exercises to the unaffected joints.
- Pulsed electromagnetic field therapy (PEMF) is known to help.
- No active movements to the affected muscles.
During the Next 24 to 48 Hours
- The pressure bandage is removed and active muscle exercises are begun.
- Stretching within the limits of pain is commenced.
- Thermotherapy: Ultrasound, short wave diathermy and TENS help to relieve pain.
- Slow rhythmic massaging helps relieve the muscle
- Non weight bearing on crutches is slowly started
- Rest of the measures is the same as above.
Between 48 and 72 hours
Apart from all the measures mentioned so far, the additional measures during this phase include:
- More vigorous active movements are encouraged.
- Deep transverse friction massage is added.
- Partial weight bearing can be permitted.
After 72 hours
All the above measures are pursued in a more vigorous manner.
- Pressure bandage is totally removed.
- Progressive resisted exercises using the Fowler technique by taking out 10 to 12 repetition maximum (RM), is practiced.
- Full weight bearing should be permitted in injuries of the lower limbs.
- After full movement is regained, the patient is allowed to walk and jog.
- Full functional activity should be regained by 4 to 6 weeks.
- The various drugs used in the treatment of muscle strain to relieve pain and muscle stiffness is depicted.
Grade Four Strain
Cause: This is usually caused by severe trauma.
Pathology
- Complete tear of the muscle.
- The fascia is tom.
- Considerable bleeding which is intramuscular and diffuse.
- Gross swelling is present.
Clinical Features
- Excruciating pain.
- Severe tenderness is present.
- A snapping sound may be heard by the patient.
- Palpable gap between the muscles felt.
- Severe loss of function.
- Active movements produced by the agonist are absent.
- Active muscle contraction is absent.
- Joint function is not lost.
- Muscle spasm is very severe.
Treatment
Surgery is advised. This involves opening the ruptured site, evacuating the hematoma and suturing the fascia sheath. Direct muscle repair is avoided.
- Compression bandage is applied and the limb is immobilized for 2 to 3 weeks.
- Active exercises to the unaffected joints.
- Slow rhythmic isometric exercises to the affected muscles.
- Non-weight bearing after 48 hours.
- The use of low frequency current (faradism) to obtain passive contraction is very useful.
- Deep heating modalities like ultrasound, etc. help.
- Rest of the measures is same as for Grade II / III injuries.
If you suffer a muscle injury(Strains) which fails to respond after a few days or continues to niggle, please contact Alliance Physical Therapy for more specific advice. For more detailed Information Call Now at: 703-205-1919
http://www.alliancephysicaltherapyva.com/