Conditions Masquerading as Sports Injury:

Not every patient who presents to the sports medicine clinician has a sports-related condition. Sports medicine, like every branch of medicine, has its share of conditions that must not be missed but appear at first to be rather benign conditions. The aim of this article is to remind you that the patient with the minor ‘calf strain‘ may, in fact, have a deep venous thrombosis, or that the young basketball player who has been labeled as having Osgood – Schlatter disease because of playing may actually have an osteosarcoma. The first part of the article outlines a clinical approach that should maximize your chances of recognizing a condition that is masquerading as a sports-related condition. The second part of the article describes some of these conditions and illustrates how they can present in the sports medicine setting.
Examination
The key to recognizing that everything is not as the first impression might suggest is to take a thorough history and perform a detailed physical examination. If the clinician has not recognized a masquerading condition from the history and examination, it is unlikely that he or she will order the appropriate investigations to make the diagnosis. For example, if a patient presents with tibial pain and it is, in fact, due to hypocalcaemia secondary to lung cancer, a bone scan of the tibia looking for stress fracture will usually not help with the diagnosis, but a history of weight loss, occasional hemoptysis and associated shoulder pain, the history of associated arm tightness and the physical finding of prominent superficial veins are more important clues to axillary vein thrombosis than would be a gray-scale ultrasound scan looking for rotator cuff tendinopathy.
If there is something about the history and examination that does not fit the pattern of the common conditions, then consider alternative, less common conditions. To be able to make the diagnosis of a rare or non-musculoskeletal condition, you must ask yourself, Could this be a rare condition or unusual manifestation? Then other options are entertained, and the appropriate diagnosis can be conceived. Thus, successful diagnosis of masquerading conditions requires recognition of a discrepancy between the patient’s clinical features and the typical pattern that one is familiar with from clinical experience.
Bone and Soft Tissue Tumors
Primary malignant tumors of bone and soft tissues are rare but when they occur it is most likely to be in the younger age group (second to third decade). Osteosarcomata can present at the distal or proximal end of long bones, more commonly in the lower limb, producing joint pain. Patients often recognize that pain is aggravated by activity and hence present to the sports medicine clinic. The pathological diagnosis of osteosarcoma is dependent on the detection of tumor producing bone and so an X-ray may reveal a moth eaten appearance with new bone formation in the soft tissues and lifting of the periosteum (Codman’s triangle) .In young patients, the differential diagnosis includes osteomyelitis. It is recommended that any child or adolescent with bone pain be X-rayed. Surgery is the preferred treatment.
Synovial sarcomata frequently involve the larger lower joints such as the knee and ankle. Patients present with pain, often at night or with activity, maybe with instability and swelling.
Synovial chondromatosis and pigmented villonodular synovitis are benign tumors of the synovium found mainly in the knee, which present with mechanical symptoms.
Osteoid osteoma is a benign bone tumor that often presents as exercise-related bone pain and tenderness and is, therefore, frequently misdiagnosed as a stress fracture. The bone scan appearance is also similar to that of a stress fracture, although the isotope uptake is more intense and widespread. This condition is characterized clinically by the presence of night pain and by the abolition of symptoms with the use of aspirin. The tumor has a characteristic appearance on CT scan with a central nidus.
Ganglion cysts are lined by connective tissue, contain mucinous fluid and are found mainly around the wrist, hand, knee and foot. They may be to a joint capsule or tendon sheath and may have a connection to the synovial cavity. They are usually asymptomatic but can occasionally cause pain and deformity.
Rheumatological Conditions
These are dealt with in greater detail in the section on multiple joint problems. Patients with inflammatory musculoskeletal disorders frequently present to the sports medicine clinic with a masquerading traumatic or mechanical condition. Low back pain of ankylosing spondylitis, psoriatic enthesopathy or early rheumatoid arthritis is common examples.
In patients presenting with an acutely swollen knee without a history of precipitant trauma or patellar tendinopathy without overuse, the clinician may be alerted to the possibility that these are inflammatory in origin. Prominent morning joint or back stiffness, night pain or extra-articular manifestations of rheumatologlcal conditions (e.g. skin rashes, nail abnormalities), bowel disturbance, eye involvement (conjunctivitis, iritis) or urethral discharge may all provide clues.
Disorders of Muscle
Dermotomyositis and polymyositis are inflammatory connective tissue disorders characterized by proximal limb girdle weakness, often without pain Dermatomyositis, unlike polymyositis, is also associated with a photosensitive skin rash in light-exposed areas (hands and face). In the older adult, dermatomyositis may be associated with malignancy in approximately 50% of cases. The primary malignancy may be easily detectable or occult. In the younger adult, weakness may be profound (e.g. unable to rise from the floor) but in the early stages may manifest only as under-performance in training or competition.
Dermatomyositis and polymyositis may also be associated with other connective tissue disorders such as systemic lupus erythematosus or systemic sclerosis, and muscle abnormality is characterized by elevated creatine kinase levels and electromyography (EMG) and muscle biopsy changes.
Regional dystrophies such as limb girdle dystrophy and facio-scapulo-humeral dystrophy may also adults. They are also associated with characteristic changes.
Endocrine Disorders
Several endocrine disorders, for example, hypothyroidism and hyperparathyroidism, may be associated with the deposition of calcium pyrophosphate in joints. Patients may develop acute pseudo gout or a polyarticular inflammatory arthritis resembling rheumatoid arthritis. X-rays of the wrists or knees may demonstrate chondrocalcinosis of the menisci or triangular fibro cartilage complex. Adhesive capsulitis or septic arthritis may be the presenting complaint in patients with diabetes mellitus and those with other endocrine disorders such as acromegaly may develop premature osteoarthritis or carpal tunnel syndrome. Patients with hypocalcaemia secondary to malignancy (e.g. of the lung) or other conditions such as hyperparathyroidism can present with bone pain as well as constipation, confusion and renal calculi. A proximal myopathy may develop in patients with primary Cushings syndrome or after corticosteroid use.
Vascular Disorders
Patients with venous thrombosis or arterial abnormalities may present with limb pain and swelling aggravated by exercise. Calf, femoral or axillary veins are common sites for thrombosis. While a precipitant cause may be apparent (e.g. recent surgery or air travel), consider also the thrombophilias such as the antiphospholipid syndrome or deficiencies of protein C, protein S, anti thrombin III or factor V Leiden.
The Claudicant pain of peripheral vascular disease is most likely to be first noticed with exercise and so patients may present to the sports medicine practioner. Remember also that arteriopathy can occur in patients with diabetes. Various specific vascular entrapments are also found, such as popliteal artery entrapment, which presents as exercise related calf pain, and thoracic outlet syndrome.
Genetic Disorders
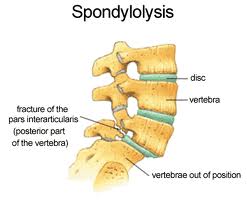
Marfans syndrome is an autosomal dominant disorder of fibril in characterized by musculoskeletal, cardiac and ocular abnormalities. Musculoskeletal problems are common due to joint hyper mobility, ligament laxity, scoliosis or spondylolysis. In patients with the Marfanoid habitus, referral for echocardiography and ophthalmological opinion should be considered as sudden carac death or lens dislocation may result. Hemochromatosis is an autosomal recessive disorder of iron handling, which results in iron overload.
Patients may present with a calcium pyrophosphate arthropathy with characteristic involvement of the second and third metacarpophalangeal joints and hook-shaped osteophytes seen on X-ray of these joints. While ferritin levels are raised in patients with hemochromatosis, it is important to remember that ferritin is also an acute-phase protein and so levels can be elevated in response to inflammatory arthropathy.
Infection
Bone and joint infections, while uncommon, may have disastrous consequences if the diagnosis is missed. Bone pain in children, worse at night or with activity, should alert the clinician to the possibility of osteomyelitis. Bone infection near a joint may result in a reactive joint effusion. Septic arthritis is rare in the normal joint. In arthritic, recently arthrocentesed or diabetic joints, sepsis is much more common. Rapid joint destruction may follow if left untreated.
Even though Staphylococcus aureus is the causative organism in more than 50% of cases of acute septic joints, it is imperative that joint aspiration for Gram stain and culture and blood cultures are taken before commencement of antibiotic treatment. Once only or repeated joint lavage may be considered in patients receiving intravenous antibiotic treatment. The immune compromised patient may present with a chronic septic arthritis. In this situation, tuberculosis or fungal infections should be considered.
Regional Pain Syndromes
Complex regional pain syndrome type 1 (formerly known as reflex sympathetic dystrophy [RSD]) is a post-traumatic phenomenon characterized by localized pain out of proportion to the injury, vasomotor disturbances, edema and delayed recovery from injury. The vasomotor disturbances of an extremity manifest as vasodilatation (warmth, redness) or vasoconstriction (coolness, cyanosis, mottling). Early mobilization and avoidance of surgery are two important keys to successful management.
Myofascial pain syndromes develop secondary to either acute or overuse trauma. They present as regional pain associated with the presence of one or more active trigger points.
Fibromyalgia is a chronic pain syndrome characterized by widespread pain, chronic fatigue, decreased pain threshold, sleep disturbance, psychological stress and diffusely tender muscles. It is often associated with other symptoms, including irritable bowel syndrome, dyspareunia, headache, irritable bladder and subjective joint swelling and pain. Fibromyalgia is diagnosed on the examination finding of 11of 18 specific tender point sites in a patient with widespread pain. Current treatment evidence is for a stepwise program emphasizing education, certain medications, exercise and cognitive therapy. Chronic fatigue syndrome has many similarities to fibromyalgia’s and may be the same disease process. It may present as excessive post-exercise muscle soreness but is always associated with excessive fatigue. Behavioral therapy and graded exercise therapy have shown promise as treatment.
At Alliance Physical Therapy we provide 24/7 access to online appointments, with most of the requests scheduled in less than 48 hours. For More Information Call Now at: 703-751-1008
http://www.alliancephysicaltherapyva.com/



 703-205-1919
703-205-1919