Sports Injuries and Its Classifications:
INTRODUCTION:
Sports medicine, like all other branches of medicine, aims at the complete physical, mental and spiritual well-being of a sportsperson. A healthy mind in a healthy body is a concept, which is more true to a sportsperson than anybody else is. Positive thinking, fair play and sportsmanship should be the hallmark of a true sportsman. We, the doctors and the therapists, aim to keep a sportsperson physically fit so that the rest of the objectives mentioned above are attained automatically.
Like in other branches of medicine so in sports medicine, prevention is better than cure. To prevent sports injuries, the first step is to ascertain whether a person choosing sports is fit to take it. An unfit person taking up sports is a sure prescription for future sports injuries. A fitness testing for those who wish to take up sports, as their career should include various relevant parameters
However, one has to remember that fitness testing is not done only at the initial stages but needs to be done repeatedly at every stage of an athlete or a sportsperson’s life. The second stage of prevention of sports-related injuries is assessing whether a sportsman is fit enough to resume the sporting activity after the initial layoff. There is nothing more dangerous than an unfit or partially fit person resuming the sporting activity. It may spell a doom to his otherwise flourishing career in sports. A sportsperson has to satisfy certain norms before he can finally be sent back to the field.
CLASSIFICATION OF SPORTS INJURIES
Among the various classifications proposed for sports injuries, the one proposed by Williams (1971) is widely used and recommended.
Williams’ Classification:
Among the Consequential Injuries
Primary Extrinsic
- This is further subdivided into:
- Human: Black eye due to direct blow.
- Implemental: May be incidental (as in blow from a hard ball) or due to overuse (blisters from oars).
- Vehicular: Clavicle fracture due to fall from cycle, etc.
- Environmental: Injuries in divers.
- Occupational: Jumper’s knee in athletes, chondromalacia in cyclists, etc
Primary Intrinsic
This could be acute or chronic.
- Incidental: Strains, sprains, etc.
- Overuse:
- Acute, e.g. acute tenosynovitis of wrist extensors in canoeists.
- Chronic, march fracture in soldiers, etc.
Secondary
Short-term: For example, quadriceps weakness.
Long-term: Degenerative arthritis of the hip, knee, ankle, etc.
No Consequential Injuries
These are not related to sports but are due to injuries either at home or elsewhere and are very not connected to any sports (e.g. slip and fall at home).
COMMON SPORTS INJURIES
Sports medicine usually deals with minor orthopedic problems like soft tissue trauma. Very rarely, there may be serious fractures, head injuries or on the field deaths. There is nothing unusual about these injuries except that a sportsperson demands a 100 percent cure and recovery while an ordinary person is satisfied and happy with a 60-80 percent recovery. The difference is because of the desire of the sports person to get back to the sport again, which requires total fitness.
The following are some of the most common sports -related injuries one encounters in clinical practice.
Upper Limbs
- Shoulder complex
- Rotator cuff injuries
- Shoulder dislocations
- Fracture clavicle
- Acromioclavicular injuries
- Bicipital tendinitis or rupture.
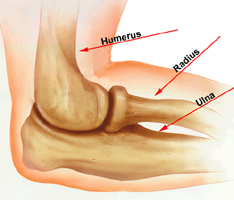
- Elbow
- Tennis elbow
- Golfer’s elbow
- Dislocation of elbow.
- Wrist
- Hand
- Mallet injury
- Baseball finger
- Jersey thumb
- Injuries to the finger joints.
Lower Limb
- Hip
- Iliotibial or tract syndrome
- Quadriceps strain
- Hip pain
- Groin pain due to adductor strain
- Knee Joint
- Jumpers Knee
- Chondromalacia
- Fracture patella
- Knee ligament injuries
- Meniscal injuries.
- Legs
- Calf muscle strain
- Hamstrings sprain
- Stress fracture tibia
- Compartmental syndrome of the leg.
- Ankle Injuries
- Ankle sprain
- Injuries to Tendo-Achilles
- Tenosynovitis.
- Foot
- March fracture
- Jones fracture
- Forefoot injuries
- Injuries of sesamoid bone of the great toe.
- Head, Neck, Trunk and Spine
- Head injuries
- Whiplash injuries
- Rib fractures
- Trunk muscle strains
- Abdomen muscle strain
- Low backache
All these injuries have been discussed in relevant sections.
Investigations
These are the same as for any ortbopedic-resared disorders and consist of plain X-ray, CT scan, bone scan, MRI, arthroscopy, arthrography, stress X-rays etc.
TREATMENT OF SPORTS INJURY
This is discussed under three headings prevention, treatment proper and training.
Preventive Measures
The best way to treat a sports injury is to prevent it from happening. Nothing is better than preventing the injury.
Treatment
Treatment of individual sports-related disorders is discussed under suitable sections. However, a mention is made here of the general principles of treatment which is applicable to all sports injuries.
General Principles
- Concept of RICEMM: This sums up the early treatment methodology of sports injuries and consists of:
R-Rest to the injured limb
I-Ice therapy
C-Compression bandaging
E- Elevation of the injured part
M- Medicines like painkiller s, etc.
M- Modalities like heat, straps, supports, etc.
- After immobilization and rest, early vigorous exercises should be commenced at the earliest to prevent muscle weakness and atrophy.
- To prevent joint stiffness, early mobilization ha s to be done first by passive movements and later by active movements. To improve the strength, resistive exercises are added.
- Unlike the conventional once a day treatment, a sportsperson needs to be seen at least 2-3 times a day.
- As mentioned earlier, allow resumption of sporting activity only after the sportsperson assumes 100 percent fitness.
- Mind training is as important as physical training. By repeated counseling, improve the psychological status of the patient to avoid depression, anxiety and negative attitudes, which may develop during the injury.
- Orthopedic and surgical treatment to be undertaken at appropriate situations.
Training
The physiotherapist has to train a sportsperson in various exercises to enable him to keep his fitness level very high. After conducting a fitness testing, the therapist has to subject an athlete to various forms of exercises to increase the endurance, strength, running, weight bearing, etc. The following are the various forms of exercises.
Measures of Relaxation
After the vigorous workout mentioned above, the sportspersons are taught methods of relaxation and body stretches. Before an athlete or a sportsperson resumes his sporting activities, a fitness testing is carried out and only then, he is allowed to take to the sports provided he is 100 percent fit.